Wheelchair Service Delivery
Part three of the provision of manual wheelchairs in less resourced settings. Published with permission of the World Health Organization. This chapter covers the structural guidelines for wheelchair service delivery systems that provide and improve access to wheelchairs. The need to provide wheelchairs together with these related services is essential. Careful planning, management and sound strategies for wheelchair provision, as well as user instruction and care are needed to facilitate the important link between the user and the wheelchair.
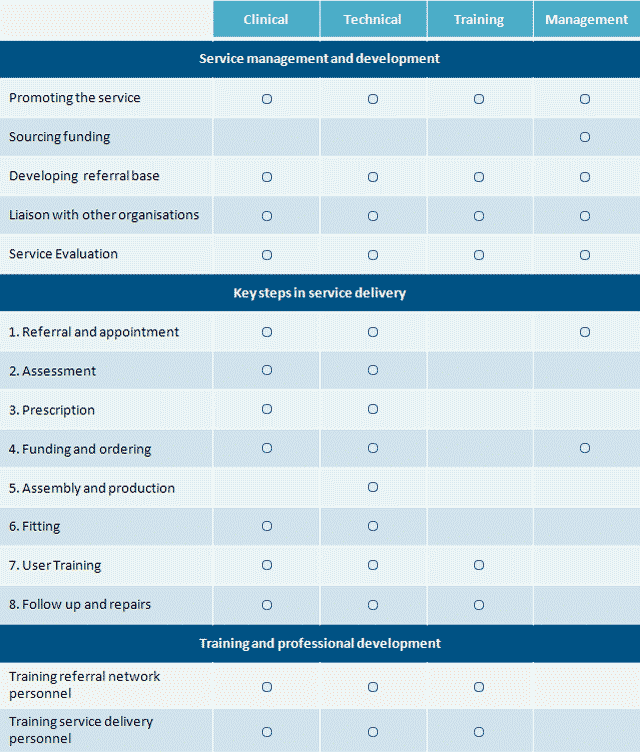
We cover all stages of the service delivery process, from referral to assessment and prescription, funding, ordering, product preparation, fitting, user training and maintenance. Including discussion of the roles of those involved in wheelchair service delivery, from manufacturers and clinicians, to technical and training personnel. Recommendations are made on monitoring, how to obtain feedback from wheelchair users, and evaluating and analyzing information on wheelchair service delivery.
- Manual wheelchair sourcing supply, manufacture, supply suggest strategies for introducing wheelchair service delivery.
- Describe basic wheelchair service delivery.
- Provide practice guidelines.
- Suggest roles for the personnel involved.
- Make recommendations on monitoring and evaluation.
Testimonial from a user in Romania, Ciprian is 25 years old and lives in Sfantu Gheorghe, Romania. Three years ago he became paraplegic after falling from a roof while at work and lost any hope that he would ever have a normal and active life again. Sometime after the accident, however, he heard about a local nongovernmental organization that provided support for users. Through the wheelchair service run by the organization, Ciprian received an active-style manual wheelchair that was fitted for him. He was also invited to participate in a peer group training camp.
Once I got there I realized that I could have an independent life. Through the peer group training, I learnt to use my wheelchair very well. I also had the chance to talk with other users involved in the programme. At the end of the camp, I was asked if I would like to become a peer group trainer. Of course, I was very happy about this chance that had just been offered to me. In January 2006, I started my work as an instructor.
Through my wheelchair, and peer training, I have recovered the independence I thought I had lost because of the injury. In addition to my peer group training work, I take part in various competitions and sports activities for people in wheelchairs. Working with people with disabilities makes me feel that I am useful again and that I finally have a normal life after I had had such a hard time overcoming the health problems brought about by the injury. — Cipran of Romania
The purpose of these manual wheelchair service delivery guidelines is to improve the way in which users receive wheelchairs and to ensure that the wheelchairs are appropriate. The implementation of the recommendations in this chapter aim to see more success stories like Cipran come true. We begin with these basic principles:
- A greater number of wheelchair services.
- Better knowledge of wheelchair service delivery among health care and social service workers.
- Better service quality delivered by existing wheelchair services.
- A greater number of appropriate wheelchairs provided to users.
- A greater number of users able to make informed decisions about the most appropriate wheelchair for them.
- A greater number of users and caregivers receiving training in the use and maintenance of wheelchairs and on how to stay healthy in a wheelchair.
- Links between users and producers, leading to producers obtaining feedback on the wheelchairs they produce.
- Coordinate efforts in the planning, implementation and support of wheelchair service delivery among stakeholders.
In the rehabilitation of a person with a spinal cord injury the provision of an appropriate wheelchair is critical. It is important that the wheelchair fits correctly and meets the user’s physical, functional and environmental needs as much as possible. This requires an approach that responds to individual needs. An effective way of meeting the individual needs of users is to promote the provision of wheelchairs through wheelchair services.
Wheelchair services provide the framework for assessing individual user needs, assist in selecting an appropriate wheelchair, train users and caregivers, and provide ongoing support and referral to other services where appropriate. In addition providers of wheelchair services will play a role in the following.
- Awareness: disseminating basic information about the needs for and benefits of using a wheelchair (this can also be done by personnel involved in community-based rehabilitation, health and education programmes as well as by disabled people’s organizations) and convincing policy-makers about the benefits of investing in wheelchair provision rather than leaving people with disabilities to survive on charity.
- Identification: using a screening tool to identify those who can benefit from available services.
- Awareness of referral networks and suppliers: promoting the role of wheelchair services, including participation in activities aimed at educating referral networks and raising the awareness of suppliers and funding agencies regarding the role and importance of wheelchair services.
- Sustainability: developing sustainable financial solutions for the continuing provision of mobility equipment through wheelchair services.
- Training: providing or supporting the training of wheelchair service personnel.
- Standards: raising wheelchair standards within the country or region through being aware of current wheelchair availability and advocating for improvements in and a greater variety of wheelchair products.
- Accessibility: supporting or facilitating the adaptation of homes (including toilets, furniture and fittings) and public buildings and places, and lobbying for a barrier-free environment.
Wheelchair Service Delivery Strategies
Wheelchair service delivery requires careful planning and management of resources. There are a number of strategies that can be employed to initiate or further develop wheelchair services. Provide wheelchairs together with services. There are different methods of wheelchair supply to meet the range of contexts in which users live. Whatever the method or structure chosen, it is important to at least deliver the essential wheelchair services.
Utilize existing personnel. It is not necessary to create a new profession to provide wheelchair services. With additional training, many health and rehabilitation personnel would be able to take on the duties required for basic wheelchair service delivery. For example, community health care workers, community-based rehabilitation workers, nurses, physiotherapists, occupational therapists, orthopedists and prosthetists could be trained to fulfil the clinical role in wheelchair services. Likewise, with additional training, skilled craftspeople, mechanics and orthotic and prosthetic technicians could fulfil the technical role.
Meet the needs of users at community level. Some aspects of wheelchair provision can be carried out in the community, through a network of community-based organizations (for example rehabilitation and health programmes) supported by a local wheelchair service delivery centre. The personnel of the community-based programmes could be trained by wheelchair service personnel in basic service delivery. This system of service delivery would best suit users who require a basic wheelchair, without modifications, postural support or pressure management care.
Users with more complex needs are likely to require the skills of personnel with greater training than can be provided to all community-level personnel. This need can be addressed by outreach services coordinated by the wheelchair service centre. If outreach services are not developed, these users would need to travel to the wheelchair service centre. However, once provided with an appropriate wheelchair, they may be supported by community-based personnel.
A wheelchair service can make use of the skills, technologies and capacities of local industries. For example, bicycle repair shops can also repair wheelchairs, and tubular furniture makers have the basic skills and knowledge to build wheelchairs.
Two Tier Wheelchair Service Approach
This shows a possible model of linking a wheelchair service centre with a number of community-based wheelchair services. To provide adequate support to the community-based centres, it may be necessary to first develop the wheelchair service centre. Alternatively, a collaborative effort between existing community based centres could work towards the development of the wheelchair service centre. In either case, the development process should be based on a needs assessment and other aspects of the local context.
The Wheelchair Service Delivery Centre
Characteristics: Centre-based. Facilities (possibly shared with existing health or rehabilitation services): clinical and user training facilities, workshop facilities. Staff: dedicated wheelchair service centre personnel trained to meet the needs of all users.
Key functions: Wheelchair service delivery for all users. Community outreach linking with community based wheelchair services and referral networks. Training, support and supervision of community based wheelchair services and personnel. Education of referral sources. Linking with education, employment and other key development sectors.
Community Based Wheelchair Services
Characteristics: Centre-based, with some wheelchair service delivery carried out entirely in the community. Facilities (shared with other community health and rehabilitation programmes): access to clinic, user training facilities, basic workshop facilities. Staff: community health and rehabilitation workers trained in basic wheelchair service delivery, supervised and supported by wheelchair service centre personnel.
Key functions: Wheelchair service delivery for users requiring basic wheelchairs without custom modifications or postural support components. Identification of users with complex needs, and referral to wheelchair service centre. Where appropriate, support of users with more complex needs for follow-up, maintenance and repair in the community. Support of accessibility, including adaptation of user’s environment such as wider doors and ramps.
Intergrating wheelchair service delivery with other departments can be established within existing rehabilitation services. Such services are already likely to have users accessing the service for health or rehabilitation needs. They would therefore already have much of the infrastructure required. Examples of rehabilitation services well suited to the integration of a wheelchair service include prosthetics and orthotics services and spinal injury centres.
Wheelchair service delivery could play a dual role, providing wheelchairs directly to users and supporting basic services in the community through partnerships with community-level programmes and organizations.
Stakeholders and Resources
Stakeholders directly involved in the planning, implementation and participation in service delivery include:
- Users and their families or caregivers.
- Government authorities, including ministries responsible for health, social welfare and education and other relevant departments and local authorities.
- Existing health and rehabilitation services (including referral networks) managed by governmental, private, nongovernmental, international nongovernmental or disabled people’s organizations.
- Supporting organizations providing technical input or funding.
- Rehabilitation personnel and their organizations.
- Wheelchair service personnel.
The resources required to implement the recommendations include:
- A reliable supply of wheelchairs that meet agreed standards.
- Access to different types and sizes of wheelchair to meet the varied needs of individual users.
- Personnel with training in wheelchair service delivery.
- Facilities (which may be shared with existing rehabilitation or health services): clinical facilities providing sufficent space for assessment basic user training and storage of wheelchairs and workshop facilities particularly where modifications to wheelchairs are offered or support is provided.
- Materials for wheelchair modifications and custom components.
- Funding to support wheelchair service delivery (products and services).
Wheelchair Service Delivery Network
In Papua New Guinea, an estimated 50 000 people need a wheelchair. Throughout 2003 and 2004, governmental health and rehabilitation organizations and national and international nongovernmental organizations developed a strategy for wheelchair provision. As a result, a pilot wheelchair service network, closely linked to the existing health and rehabilitation services, was set up.
The wheelchair service delivery network consists of a “regional wheelchair service” supporting four “satellite wheelchair services”. The regional service is based at the National Orthotics and Prosthetics Service in Lae. At the regional service, technical personnel from the National Orthotics and Prosthetics Service team and physical therapy personnel from Lae’s Angau Hospital together carry out assessment, prescription, fitting, user training and follow-up. The National Orthotics and Prosthetics Service provides repair services for users. This mixture of clinical and technical facilities has made the setting up of the wheelchair service relatively easy, and the recent provision of dedicated premises for the service has given it a stronger identity.
Two of the satellite services are based in local hospitals, one in a local prosthetic unit and one in a local community based rehabilitation service. The community-based rehabilitation link with each service is strong. The community based rehabilitation networks provide excellent referral, and the personnel work with hospital-based personnel to provide users with a wheelchair.
Training in basic wheelchair service delivery for all of the clinical and technical personnel involved in the service network was provided over two weeks by the international nongovernmental organization Motivation. Further support for both clinical and technical personnel for one year was provided by a volunteer physiotherapist.
The network has the capacity to provide 25 wheelchairs per month. This is still not sufficient to meet the needs in Papua New Guinea. However, through the success of this pilot exercise in using existing services and personnel, much has been learnt about the role of wheelchair services. In future, all stakeholders are keen to see the establishment of more satellite services, as well as an increase in the capacity of the network to meet the needs of users with more complex needs.
Steps in Wheelchair Service Delivery
Wheelchair services are commonly delivered in a sequence of steps. A summary of eight (8) key steps typically involved in wheelchair service delivery are as follows:
- Referral and appointment The system of referral will depend on existing services in the country. Users may self-refer or be referred through networks made up of governmental or nongovernmental health and rehabilitation workers or volunteers working at community, district or regional level. Some services may need to actively identify potential users if they are not already receiving any social or health care services or participating in school, work or community activities.
- Assessment Each user requires an individual assessment, taking into account lifestyle, vocation, home environment and physical condition.
- Prescription (selection) Using the information gained from the assessment, a wheelchair prescription is developed together with the user, family member or caregiver. The prescription details the selected wheelchair type, size, special features and modifications. Also detailed is the training the user needs to effectively use and maintain the wheelchair.
- Funding and ordering A funding source is identified and the wheelchair is ordered from stock held by the service or from the supplier.
- Product preparation Trained personnel prepare the wheelchair for the initial fitting. Depending on the product and service facilities, this may include assembly, and possible modification, of products supplied by manufacturers or production of products in the service workshop.
- Fitting The user tries the wheelchair. Final adjustments are made to ensure the wheelchair is correctly assembled and set up. If modifications or postural support components are required, additional fittings may be necessary.
- User training The user and caregivers are instructed on how to safely and effectively use and maintain the wheelchair.
- Follow-up, maintenance and repairs Follow-up appointments are an opportunity to check wheelchair fit and provide further training and support. The timing depends on the needs of the user and the other services that are available to them. The service may also offer maintenance and repairs for technical problems that cannot be easily solved in the community. It is appropriate to carry out follow-up activities at the community level as much as possible. If the wheelchair is found to be no longer appropriate, a new wheelchair needs to be supplied starting again from step 1.
Understanding Individual User Needs
When planning wheelchair service delivery, it is important to recognize that each user has a unique set of needs. These needs can be categorized as:
- Physical: the user’s health situation and postural and functional needs.
- Environmental: where users live and where they need to use the wheelchair.
- Lifestyle: the things users need to do in the wheelchair to lead their chosen way of life.
Physical Needs. Some users will have a more complex mix of physical needs than others. Users with spinal cord injury, postural deformities, reduced skin sensation and problems with muscle tone (for example spasticity) will require an assessment conducted by personnel with appropriate skills and knowledge. These users will also require more frequent follow-up and support. Here we consider some postural needs of users related to their need for personnel skill and support:
Users of manual wheelchairs without modifications. Children or adults who can sit well without any postural deformities or abnormalities.
Needs: Mobility and postural support for comfort, function and the prevention of postural problems associated with permanent wheelchair use. Mobility and postural support provided through a well-fitted wheelchair and seat cushion.
Users of manual wheelchairs with supportive seating. Children or adults with mild to moderate postural deformities or tendencies. If unaddressed, these deformities will limit comfort, health and function.
Needs: Mobility and postural support to stabilize posture for comfort, function and prevention of further postural problems. Supportive seating provided through individual modifications to a basic wheelchair, or a specialized seating system.
Users of complex supportive seating and mobility equipment. Children or adults with complex, fixed postural deformities. Even with support, many cannot sit normally.
Needs: Mobility and individually prescribed and customized wheelchairs to provide postural support and accommodate fixed deformities. Increased need of skill and support and accommodate fixed deformities.
Environmental and lifestyle needs. These factors require consideration during the assessment. They will influence the choice of a wheelchair, based on performance characteristics, durability and other features. How many users require more than basic wheelchair provision?
In a survey of 147 users conducted at the Western Cape Rehabilitation Centre in South Africa in 2006, it was found that 58% of users required some form of wheelchair modification or basic postural support. Some 22% required complex postural support, while only 20% were able to use a basic manual wheelchair without any modification. A supervisory chief physiotherapist states:
Since our service began, we have found that many users need more than just a basic wheelchair. Many have deformities from living so long without a wheelchair and now need their wheelchair modified so that it fits them. We also have more and more children with cerebral palsy coming to us, and they need wheelchairs with extra postural support. — WCRC Chief Physiotherapist
Good Practice in Wheelchair Service Delivery
This section covers planning and initiating wheelchair service delivery and evaluating existing services. Recommendations are presented in nine areas: good practice in overall service and for each of the eight key steps in wheelchair service delivery. Good practice in wheelchair service delivery includes the following:
- Wheelchair services recognize users as clients of the service and adopt a “client-centred approach”. This means, inter alia,that: Users receive information about the process the wheelchair service will use to provide a wheelchair, and the rights and responsibilities of the user in this process. Users are actively involved as members of the service team in all steps leading to the provision of their wheelchair. Services actively collect feedback from users about their opinion of the service and how it may be improved.
- The service is equally accessible to all users, regardless of gender, age, ethnicity, religion or social status.
- The service has personnel trained in its clinical, technical and training roles, who work closely with users to provide advice, assessment, prescription, fitting, training and follow-up.
- The service has a designated service manager or coordinator.
- A referral network is in place.
- The service is well integrated with other rehabilitation and health services.
- Services are knowledgeable about the range of wheelchairs available locally.
- Services are able to offer more than one type of wheelchair, giving the user a choice based on the assessment.
- Wheelchairs are sourced from a range of suppliers, including local and international, depending on their appropriateness and affordability.
- Services carry out quality control to ensure that every wheelchair is assessed for safety before the user tries it and for safety and correct fit before each user leaves the workshop or rehabilitation centre with the wheelchair.
- Repair services are available to provide continuing support to users.
- Services identify local needs and measure their effectiveness in meeting these needs through regular monitoring and evaluation.
- Services promote teamwork between clinical and technical personnel in providing service to users.
Referrals and Appointments
Objective: The objective of good practice in referrals and appointments is to ensure that users have equitable access to wheelchair service delivery, to increase the efficiency and productivity of the service, and to minimize waiting lists.
Referral System: This pertains to the way in which users access the service. This may be through “self-referral”, whereby users contact the service directly, or through a “referral network”, whereby users are referred by another organization.
Appointment System: This refers to the method of establishing appointment times with users for assessment and prescription, fitting, basic user training and follow-up. The most common method is to list appointment times in a service diary, which are then filled as users are referred. The benefits of an appointment system include reduced waiting times and increased work efficiency.
Waiting Lists: Where there is high demand for the wheelchair service, a waiting list will need to be established. Users on the waiting list can be offered an appointment as the service works through the list. The administration of appointments will depend on the context.
Good Practice in Appointment and Referral Systems
- When a user is referred to the service, a file is established and an appointment is made or the user is put on the waiting list.
- Services provide training for referral network personnel to increase their awareness of wheelchair service delivery and to show them how to refer users to the service.
- Services develop and distribute a form for referral network agencies to complete when referring users.
- Services use clear guidelines to prioritize appointments. This is particularly important where there are waiting lists. Examples of high-priority users include those with a terminal illness and those at risk of developing life-threatening secondary complications such as a pressure sores.
- Services set targets and measure their performance in relation to the number of referrals, the length of time between referral and appointment, and reduction of waiting lists.
- Services have a screening procedure to minimize the scheduling of inappropriate referrals.
Assessment
The objective of good assessment practice is to accurately assess the needs of each individual user in order to prescribe the most appropriate wheelchair available.
Every user requires an individual assessment, carried out by a person or persons with the appropriate skills. The assessment should be holistic, taking into account the lifestyle, living environment and physical condition of the user. It is important that the user and, if appropriate, the family are fully involved in the assessment. Depending on the complexity of the needs, an assessment can take up to two (2) hours.
- Assessments are carried out in a private, quiet and clean space. This may be a dedicated space within the wheelchair service, at another health care or community facility, or at the user’s home.
- Assessments are carried out by trained personnel. Culture, age and gender sensitivity while carrying out assessments increases credibility and acceptability.
- Equipment for the assessment is readily available, including an assessment bed (plinth, mat, table), measuring tape, device for measuring angles (goniometer), foot blocks and infection control supplies.
- Assessment takes into consideration the user’s physical condition; home, school, work and other environments where the wheelchair is used; lifestyle; size and age.
- Assessments are clearly documented on an assessment form and filed for future reference.
- Where a service is unable to meet the user’s needs owing to the lack of an appropriate product or personnel with sufficient skills, the service either; refers the users to another service that is staffed and equipped to service the user, hosts outreach visits of more qualified personnel or, documents the user’s needs to help build a picture of unmet need to guide future service development.
Prescription
The objective of good prescription practice is to match the needs of the user, as identified through the assessment, with the most suitable wheelchair available. Wheelchairs need to be available in different types and sizes and with different options. The prescription (or selection) represents the process of matching the needs of the user with the most suitable available wheelchair. The completed prescription form is a full description of the wheelchair required and selected by the individual user.
- Users are given the opportunity to see and, where possible, try samples of wheelchairs, cushions and postural support components. This assists users and personnel together in selecting a wheelchair and the necessary features.
- The importance of features is prioritized to help to make the most appropriate choice from what may be a limited range of available wheelchairs.
- Each wheelchair prescription is documented, either on the assessment form or on a dedicated prescription form. The prescription details; the type and size of wheelchair, any additional components required (for example pressure-relief seat cushion), any modifications or custom comments required and, the information or skills the user needs to know, or be able to perform, before leaving the service with a new wheelchair.
- Wheelchair service personnel are given time to write up assessment and prescription notes immediately after each appointment.
- Services give users an estimate of when their wheelchair will be ready (depending on funding, see below). Where possible, an appointment for the user’s fitting is made at the time the prescription is made.
Funding and Ordering
Objective: The objective of good practice in funding and ordering is to order or procure the selected wheelchair for the user, as early as possible.
Funding: Following prescription, it is possible to closely estimate the cost of the product being recommended. For most services, it will be essential to ensure a funding source has been identified before an order can be placed for equipment. Wherever possible, this should be in the hands of administrative rather than clinical or technical personnel.
Ordering: When not in stock, wheelchairs need to be ordered from an external supplier or procured from the wheelchair service workshop, which usually maintains a stock of different sizes and types of wheelchair.
- If a wheelchair is not immediately available, services inform the user when the wheelchair will be ready for fitting.
- Services maintain a stock of wheelchairs and components to ensure faster delivery times.
- Services encourage suppliers to develop clear order forms and procedures.
- Services agree with suppliers on delivery times and aim to minimize delays.
- Services ensure ordering is completed within two working days of completing the user’s prescription, provided that funding is in place.
- Services have a system in place to monitor pending orders from suppliers.
- Services have a system for providing feedback to suppliers about quality issues.
Product Preparation
The objective of good practice in product preparation is to prepare the wheelchair for the fitting, including modifications or custom postural support components. Good practice in product preparation include:
- Each wheelchair being prepared is labelled with the user’s name and a serial number or bar code.
- Modifications to wheelchairs (permanently altering the frame or a component of the wheelchair) are carried out only by personnel with the appropriate knowledge and skills, since any such modification may have structural and functional implications.
- The production and installation of custom seating systems or individual postural support components should be carried out by personnel with the appropriate knowledge and skills. This work should also be done in close collaboration with the assessment personnel.
- All mobility equipment is checked for quality and safety before the user tries it.
Fitting
The objective of good practice in fitting is to ensure that the selected wheelchair has been correctly assembled and to make final adjustments to ensure the best fit. Fitting is a critical step. At the fitting, the user and clinical and technical personnel ensure that the wheelchair fits correctly and supports the user as intended. A fitting may take between 30 minutes and 2 hours or more, depending on the complexity. During fitting, the user and competent personnel together check that:
- The wheelchair is the correct size.
- The wheelchair is correctly adjusted for the user.
- Any modifications or postural support components are fitting correctly.
- The wheelchair meets the user’s mobility and postural support needs and minimizes the risk of the user developing secondary deformities or complications.
- All users have their wheelchair individually fitted by personnel trained to do so.
- Whenever possible, fitting is carried out by the same personnel that assessed the user.
- The fit of the wheelchair (including any seating or postural components) is first assessed with the user sitting in the stationary wheelchair. When the fit is acceptable, it is then further assessed while the user self propels or is pushed.
- If the wheelchair fit is not acceptable, further adjustments are made. If an acceptable fit cannot be achieved, alternative equipment or a reassessment may be necessary. The wheelchair cannot be provided to the user until the fit is acceptable.
- There is provision for more than one fitting appointment for users with more complex needs, such as those with postural deformities.
Training of Users Families and Caregivers
The objective of good practice in training is to ensure that all users are given the information and training they need to be able to use their wheelchair safely and effectively. Key areas of training include:
- How to transfer in and out of the wheelchair.
- How to handle the wheelchair.
- Basic wheelchair mobility.
- How to stay healthy in the wheelchair, for example prevention of pressure sores.
- How to look after the wheelchair and cushion and, if appropriate, dismantle and reassemble the wheelchair.
- Who to contact in case of problems.
- A user training checklist is completed together with the user, covering the skills the user needs to have in order of priority. The checklist is used by the trainer, and as each skill is taught and demonstrated by the user it is checked off.
- Where possible, peer trainers (active users with strong wheelchair skills and training in how to teach and support other users) provide basic user training, with supervision by clinical personnel.
- Wheelchair services link closely with any user groups in the community, providing peer training to strengthen training given at the service.
- Written or visual materials, including pamphlets or posters in local languages, are used to assist the training of users.
Follow-up Maintenance and Repair
The objective of good practice in follow-up, maintenance and repair is to evaluate the effectiveness of the wheelchair in maximizing the user’s functioning, comfort and stability, and to ensure that the equipment has been maintained appropriately and is in good condition. Follow-up should include a review of:
- How well the wheelchair has worked for the user.
- Any problems the user has had in using the wheelchair.
- The wheelchair’s fit, in particular checking that the wheelchair is providing good postural support for the user.
- The user’s skills, and whether further training is required.
- The condition of the wheelchair and whether any adjustments or repairs are required.
- The user’s ability to care for and maintain the wheelchair, and whether any further training is required.
The frequency of follow-up will depend on the individual needs of the user. Some users should be followed up more frequently than others. As a guide, follow-up appointments are usually made within six months of receiving a wheelchair. Basic wheelchair repair work can often be done locally at bicycle or car repair workshops.
- Whenever possible, all members of the wheelchair service team are involved in follow-up appointments. This includes clinical, technical and training personnel.
- The frequency of follow-up is determined by the individual needs of the users.
- Follow up appointments are given as a priority to users in the following categories: children (whose needs change as quick as they grow), users at risk of developing pressure sores, users who have a wheelchair with postural support modifications or additions, users or family members or carers who have difficulty following the basic training given at the service.
- Services use follow-up appointments as an opportunity to gather feedback from the user to help evaluate the quality of the service provided.
Manufacturers or Suppliers
Wheelchair services usually receive wheelchairs from manufacturers or suppliers. The scope of these guidelines does not allow a discussion of all production and supply personnel, but a few points are made here concerning managers and technical production personnel.
Management: As well as day-to-day management, managers of wheelchair production facilities are responsible for design selection and production quality. It is therefore important that managers receive feedback from users and wheelchair services about how well their wheelchairs meet their needs.
Technical production personnel: Technical production personnel are concerned with the technical side of wheelchair production. They are not necessarily involved in the fitting or modification of wheelchairs for individual users. This differs from technical personnel in wheelchair services, who are involved in the assembly, modification and fitting of wheelchairs for specific individuals. Nevertheless, some technical personnel, typically those in smaller workshops, may be involved in both the manufacture and fitting of wheelchairs. The term “technical production personnel” as used in these guidelines is limited to wheelchair manufacturers and does not include the provision of services to individual users.
Referral Networks
Referral networks play a crucial role in wheelchair service delivery. Well-functioning referral networks help to ensure services are accessible to users. Referral networks may consist of health and rehabilitation personnel or volunteers working at community, district or regional level.
The importance of a strong link between specialist services and rehabilitation or health care programmes is stressed in a joint statement of the International Society for Prosthetics and Orthotics and the World Health Organization.
Wheelchair services are an example of a specialized service that cannot always be fully provided within every community. In developing countries, the majority of those people with disabilities live in rural areas and find it difficult to access rehabilitation services, which are often restricted to large cities. Health and rehabilitation workers therefore need to play a proactive role in ensuring that people living in rural areas can also access wheelchair services without difficulty. The role of referral networks in wheelchair service delivery can include:
- Identifying and referring people requiring wheelchairs.
- Liaising between the users, their families and the wheelchair services to facilitate assessment, fitting and follow-up.
- Reinforcing wheelchair service training such as pressure sore prevention, prevention of secondary complications, wheelchair maintenance and mobility skills.
- Providing support, advice and possibly assistance in adapting the user’s home environment.
- Encouraging measures to facilitate accessibility in the community.
- Providing information to the wheelchair services about the acceptability and use of prescribed wheelchairs.
- Assisting the user to arrange repairs.
- Promoting the benefits of wheelchairs.
Wheelchair Service Delivery Personnel Roles
Wheelchair service personnel carry out managerial, clinical, technical and training duties. These roles may be fulfilled by personnel from a range of training and educational backgrounds. They may also overlap: in a small service, for example, one person could carry out both the clinical and technical roles. In another scenario, one person could carry out the clinical, training and management roles with the support of a part-time technician.
At times, particularly when working with users who have complex needs, personnel may draw on the expertise of other specialists such as occupational therapists, physiotherapists, speech and language therapists, paediatricians, neurologists, physiatrists, orthotists, prosthetists and orthopaedic specialists.
Management Role: For a wheelchair service to operate effectively, a designated manager is critical. The manager ensures a framework is in place to enable the wheelchair service to operate. This includes adequate staffing, facilities, funding, products, referrals and appointment systems. Managers also play a key role in promoting wheelchair services. The manager therefore requires a thorough understanding of wheelchair service delivery in addition to general management skills. The duties of wheelchair service managers should include.
- Building awareness of wheelchair service delivery among all stakeholders.
- Developing a referral network through promotion of the wheelchair service and its functions.
- Organizing training opportunities for referral network personnel.
- Ensuring the service is accessible to all users within the service area, including women, children and minority groups.
- Managing waiting lists.
- Identifying and securing sources of funding to support the service.
- Facilitating the development and training of service personnel.
- Evaluating the effectiveness of the service in meeting users’ needs.
- Continuously improving service quality.
- Developing links with disabled people’s organizations and community-based rehabilitation programmes.
- Asssisting in the formation of wheelchair users’s groups.
Clinical Role: Clinical personnel work directly with the user in assessment, prescription, fitting and follow-up. Ideally, the clinical personnel work closely with technical personnel, particularly on prescription and fitting. The main duties of clinical personnel include:
- Wheelchair service delivery, following the eight-step process listed earlier.
- Quality control to ensure equipment is adjusted correctly and is safe for each user.
- Training users in mobility and health issues, or supervision of such training provided by a trainer.
- Follow-up with users to ensure that equipment continues to be appropriate to their needs.
- Record keeping and documentation.
- Education of referral network personnel.
- Keeping up to date with the range of available wheelchairs.
- Participation in overall service evaluation.
Technical Role: Technical personnel ensure that the technical requirements of the prescription are met through the correct assembly or modification of the wheelchair. Technical personnel have direct contact with users, at least in the prescription and fitting stages. When working with a user who requires modifications or postural support, it is increasingly important that technical personnel are directly involved in the user’s assessment, fitting and follow-up. The main duties of technical personnel include:
- Assembling or preparing wheelchairs according to prescription.
- Making or assembling modifications or custom postural support.
- Training users in wheelchair maintenance and basic repair, or supervising such training provided by a trainer.
- Ensuring that each wheelchair and any modifications are technically safe before each fitting and before the user leaves the service with the new equipment.
- Keeping records and documentation.
- Following up users to ensure equipment continues to be appropriate.
- Facilitating maintenance and repairs of wheelchairs and associated equipment.
- Participating in overall service evaluation.
Training Role: One of the key steps in wheelchair service delivery is basic skills training for wheelchair users. The bulk of the training may be fulfilled by clinical or technical personnel or by dedicated trainers. They also provide users with the necessary advice on maintaining their wheelchair. Experienced, well trained wheelchair users (“peer trainers”) are useful in training other users.
Provided with the right resources and training, peer trainers may have some advantages over trainers who are not users. Such advantages include an ability to empathize and to draw on first-hand experience. For those receiving a wheelchair for the first time, there is added value in training given by a peer trainer. By working with peer trainers, users are better able to recognize their own potential. The main duties of trainers include:
- Training users and caregivers, individually or as a group, in: transferal in and out of the wheelchair, wheelchair handling, basic wheelchair mobility, health issues specific to wheelchair use (pressure sore prevention, etc.), wheelchair maintenance.
- Participating in routine and more intensive follow-up for those users at risk, or who require additional training and support.
- Educating referral network personnel.
- Participating in service evaluation, focusing on the needs of users.
In addition, trainers could become involved in:
- Activities to promote the wheelchair service.
- Liaison with disabled people’s organizations and community-based organizations.
- Referral of users to relevant community programmes such as disabled people’s organizations, vocational schemes and peer group training.
For 11 years now, the Motivation Romania Foundation (MRF) based in Bucharest has provided peer training. The MRF wheelchair service and peer training programme is based on the principle that all wheelchair recipients should undergo peer training (including, but not limited to, wheelchair skills) to maximize their independence. The peer training team currently consists of four users and a physiotherapist. Each year, some 160 users access the peer training programme, which includes:
- Training in wheelchair skills
- Individual and group discussions, in which users can talk about the challenges they have faced and try to find solutions together.
- Provision of information, for example about dealing with health problems.
- Participation in sports and social activities to facilitate the development of outgoing, people-oriented attitudes and prevent isolation.
Peer training is carried out at the MRF centre and through regular peer training camps. Peer trainers are recruited from among former recipients of peer training. They receive training in teaching and counselling from experienced peer group trainers, thus enabling them to take on the role themselves.
The costs of the peer training programme are covered by the Romanian Ministry of Labour and Social Protection, the National Authority for People with Disabilities, and national and international donors.
An overview of the clinical, technical, training and management duties of wheelchair service personnel.
Monitoring and Evaluation
The need to measure performance. Monitoring and evaluation of a wheelchair service can help identify those areas that are successful and those that can be improved. Monitoring is the regular ongoing collection and analysis of information to track the quality and effectiveness of the wheelchair service. Evaluation refers to an overall evaluation, usually conducted over a short period of time. Evaluations are often carried out annually or sometimes biannually.
Information gained through regular monitoring is often used as part of an overall evaluation. It is recommended that services establish a system for regularly monitoring the service, and conduct annual overall evaluations to assess service performance and impact. Monitoring and evaluation can provide important information that enables services to:
- Improve the quality of services and products.
- Improve service processes such as referral, appointments and follow-up.
- Contain costs by increasing efficiency.
- Demonstrate the benefits of wheelchair service delivery for users.
- Demonstrate the effectiveness of the service.
- Identify and quantify unmet needs.
- Plan further development of the service.
- Allocate resources appropriately.
- Justify current and proposed service funding.
- Develop stronger partnerships with service recipients.
- Enhance credibility and funding opportunities.
Monitoring
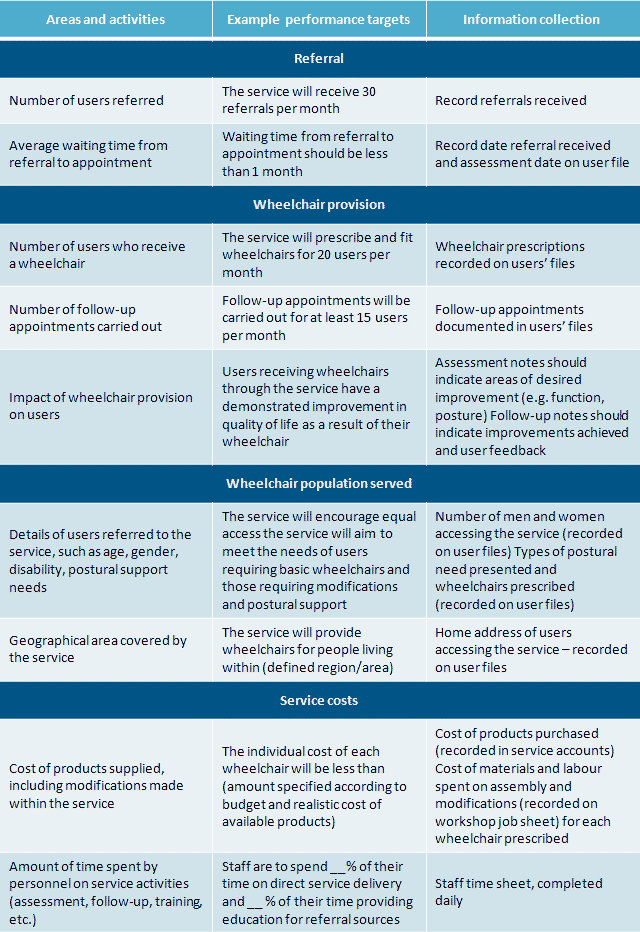
Regular monitoring can be established as follows:
- Identify the areas and activities of the service that should be routinely monitored. Examples are the rate of referrals, waiting times, the number of users receiving wheelchairs, the types of wheelchair prescribed, the number of follow-ups and the level of user satisfaction.
- Set “performance targets” for these areas and activities. A performance target is a statement of how well the service would like to perform in that area. This may often be linked to funding. For example, funding may have been provided to the service based on agreed objectives or targets. Performance targets should be realistic, taking into account the resources available.
- Identify the information that needs to be collected in order to be able to monitor service performance for each area – and how it will be collected. Ideally, gathering information should be part of the service’s normal record keeping, and should thus require very little additional work by service personnel.
Now we visit an example of service areas that could be monitored, performance targets, and ways to collect information for each service area. It is important to note that the performance targets are examples only; actual targets need to be worked out according to the resources available to each service. Examples of service areas that could be monitored, performance targets, and ways of collecting information:
Feedback from users: In addition to the routine collection of monitoring information, it is recommended that services establish methods of regularly gathering feedback from users and their families. There are several ways in which such feedback can be gathered.
- A few questions about the service can be formulated and put to users after they have received their wheelchair.
- A short questionnaire can be developed, asking users for their thoughts on the performance of the service. This could be offered to every user or to a specified number of randomly selected users each month.
- Users can be encouraged to write down their impressions of the service and post them in a “feedback box”. Feedback can be anonymous, thus allowing people to feel more comfortable about providing honest feedback. It is important to note that this type of system is open only to those with a sufficient level of literacy, and should therefore not be the only method used to gather feedback.
Analysing the collected information. The information collected through regular monitoring and user feedback will be most useful if it can be centrally stored and organized. A basic database can be very useful for this where computers and personnel are available. Alternatively, information can be organized and analyzed manually.
Once information is organized, it is possible to measure how the service is performing against the performance targets. A regular analysis of information can be used to identify problems and action can be implemented to solve the problems. For example, if fewer referrals than expected are being received, a service may choose to contact all referral sources to remind them about the service or offer additional training.
Evaluation
An overall evaluation is more comprehensive than ongoing monitoring. An evaluation provides an overview, highlighting the service’s strengths and weaknesses. Previous evaluation reports can be used as a basis for subsequent evaluations.
Service evaluations can be carried out externally or internally. An external evaluation involves having one or more people from outside of the service carrying out the evaluation. This can be useful, as external evaluators will view the service from a different perspective. Internal evaluations can be carried out by one or more personnel who have been designated the responsibility to gather and analyse the necessary information. The use of computers in data collection, programme monitoring and follow-up will facilitate the evaluation of service provision.
Suggestions for gathering evaluation information for some key service areas.
Quality of service delivery. The good practice recommendations made in Section 3.3 of these guidelines can be used as criteria to assist in evaluating the quality of service delivery.
Users served and the intervention they received. Information from ongoing monitoring should enable evaluators to quantify the number of users provided with a wheelchair, training and follow-up; the different types of wheelchair provided; and the number of users with needs that could not be met by the service. A thorough evaluation would also include information on users accessing the service, including age, gender, ethnicity, disability and home location.
Cost of service, including cost of products and service delivery. Information from ongoing monitoring should enable evaluators to review and summarize the cost of the service. An audit of accounts may also be used to determine the cost of products and services.
Staffing, numbers of personnel and their roles and competences. Evaluators can assess numbers and roles of personnel by talking to service management or reviewing personnel records. Staff competences can be assessed by observing personnel carrying out their duties. Good practice recommendations=, the personnel roles, and the clinical competences, are criteria to assist in evaluating personnel competence. Staff educational records should be reviewed to help determine competences and professional development. Feedback from users and individual interviews with personnel can help to identify strengths and weaknesses in the staffing structure.
Facilities and equipment available to the service. Evaluators can assess the suitability of facilities and equipment by observing the service in practice. Feedback from users and individual interviews with personnel can help to identify any strengths and weaknesses in service facilities.
Impact on users and their families. Information may be gathered from users and their families on the impact of the service. Measures can include increased participation in family or community activities (for example education, employment in or outside of the home, participation in social activities) and increased earning potential of wheelchair users or their families. Methods of gathering information include the following:
- Evaluators may review assessment and follow-up forms. Assessment forms can provide information about users and their families before they receive a wheelchair through the service. Follow-up reports can provide information about how the service has affected the lives of the user and his/her family.
- Home visits will enable evaluators to meet the users of the service and see for themselves what impact there has been. Home visits may provide additional information not gained through a follow-up appointment carried out at the service.
- A detailed survey may be developed to assess the service impact on the quality of life of users, including participation in school, employment and other activities.
- Users (and family members) may be gathered as a focus group to provide evaluators with information about how they believe the service has affected them.
Conclusions
Wheelchairs need to be provided together with services. Existing rehabilitation personnel can be utilized to provide wheelchair services. Integrating wheelchair services with existing health or rehabilitation services is recommended. Where possible, the needs of users should be met at community level. Wheelchair services facilitate the assessment of individual user needs, provide an appropriate wheelchair, train users and caregivers, and provide ongoing support and referral to other services.
Each user has a unique set of physical, environmental and lifestyle needs. Groups of personnel involved in wheelchair service delivery include manufacturers and suppliers, referral networks and service personnel. The main roles of service personnel are managerial, clinical, technical and educational. Peer trainers play an important role in wheelchair provision. Wheelchair provision should be regularly monitored and evaluated, especially in helping to identify those areas that are successful and those that need to be improved.
Resources
- Rushman C, Shangali HG.Wheelchair service guide for low-income countries. Moshi, Tanzanian Training Centre for Orthopaedic Technology, Tumani University, 2005.
- Sheldon S, Jacobs NA, eds. Report of a Consensus Conference on Wheelchairs for Developing Countries, Bangalore, India, 6–11 November 2006. Copenhagen, International Society for Prosthetics and Orthotics, 2007 http://homepage.mac.com/eaglesmoon/WheelchairCC/WheelchairReport_Jan08.pdf, accessed 8 March 2008).
- McCambridge M. Coordinating wheelchair provision in developing countries. In: Proceedings of the RESNA 2000 Annual Conference: Technology for the New Millennium, Orlando, Florida, 28 June – 2 July 2000. Atlanta, GA, RESNA, 2000:234–236.
- The manual wheelchair and its use. Stockholm, Swedish Institute of Assistive Technology, 1990 (In Swedish).
- Oderud T. Design. In: Report of a Consensus Conference on Wheelchairs for Developing Countries, Bangalore, India, 6–11 November 2006. Copenhagen, International Society for Prosthetics and Orthotics, 2007.
- The relationship between prosthetics and orthotics and community-based rehabilitation. A joint ISPO/WHO statement. Copenhagen/Geneva, ISPO/WHO, 2003 http://www.who.int/disabilities/technology/po_services_cbr.pdf, accessed 10 March 2008).
- Helander E. Prejudice and dignity: An introduction to community based rehabilitation, 2nd ed. New York, United Nations Development Programme, 1999
- Empowering the rural disabled in Asia and the Pacific. Rome, Food and Agriculture Organization of the United Nations, 1999 http://www.fao.org/sd/PPdirect/PPre0035.htm, accessed 10 March 2008).
The people who provide wheelchair assessment to the people who are in need of the help are really good. Thanks for sharing this blog.
It is really an informative and knowledgeable blog for the people who are unfit and need wheelchair assessment.