A wheelchair made by BMW so valuable it must be kept under guard are two of the new weapons in Rio Paralympians’ unending race for a competitive advantage.
Category: Spinal Cord Injury Articles
Informative medical information on spinal cord injury hospitalization, wheelchair life, and living with a disability from people who have been there.
Research finds poor heart health after a spinal cord injury. Ongoing damage to spinal cord nerves increases risk of poor heart health.
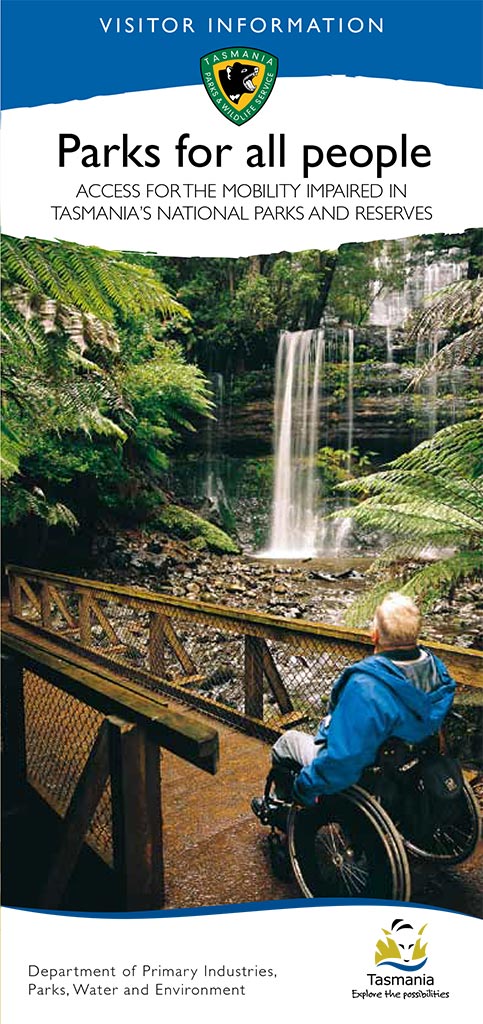
National parks and reserves around Tasmania that offer the best, and most accessible, facilities and recreational opportunities for people who are mobility impaired. A TrailRider (all-terrain wheelchair) is available at Cradle Mountain, Mount Field and Freycinet national parks for visitors with impaired mobility.
Creating 3D wheelchair model animation is easy with so many user friendly programs available these days. You no longer need a degree in kinetics to easily create realistic animations. I explained how to set up some simple 3D wheelchair models previously using free 3D software Daz3D. Now here are a few 3D wheelchair model animations ….



Recent Comments