After losing her brother and becoming a paraplegic in a horrific motor vehicle accident Sarah Casteel has gone on to become a world ranked wheelchair tennis champion. With a mean top-spin backhand the inspiring Sarah Casteel has her eyes set on the London Paralympics 2012.
Tag: disability employment
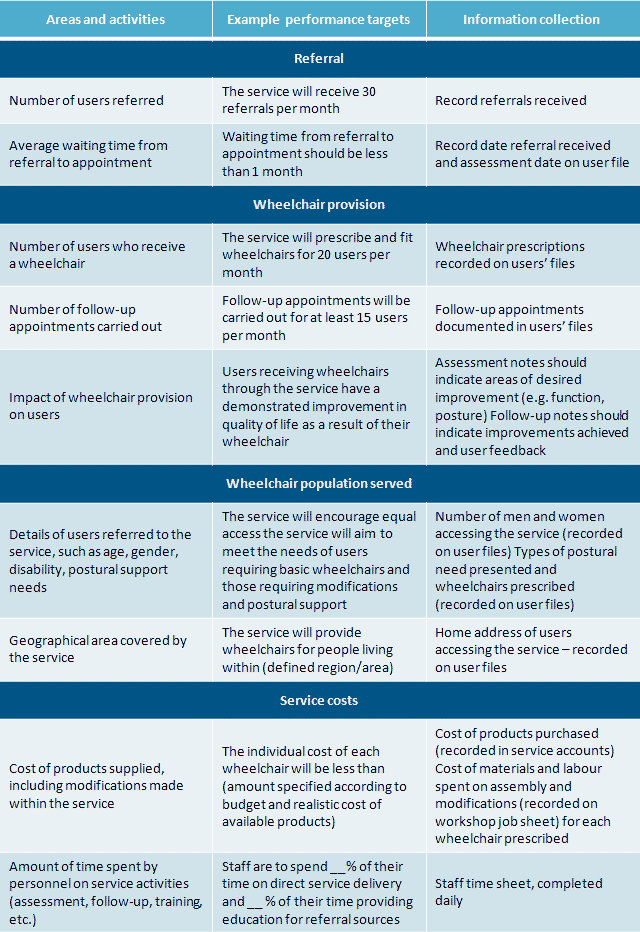
Guidelines for wheelchair service delivery systems that provide and improve access to manual wheelchairs. Great strategies for wheelchair provision, as well as user instruction and care. The important link between the user and the wheelchair.
This is the story of how I met Jeff and our first date together. My boyfriend doesn’t mind dating paraplegic girls. I use a wheelchair, leg braces and crutches because I’m paralyzed from my waist down. We really hit it off on our first date. I guess it’s hard for some men to commit to a relationship with a handicapped girl. Jeff seems to look past my disability though.
A Carlos Brooks film released by Magnolia Pictures in 2008, Quid Pro Quo stars Nick Stahl as Isaac Knott, a paraplegic radio reporter who dares follow the beautiful complex Fiona played by Vera Farmiga into the secretive world of self harm through wheelchair envy.



Recent Comments