11.5 Following primary and secondary hospital examinations a spinal cord injury is often diagnosed as a type of syndrome and a prognosis of long term expected outcomes is given. It’s important to remember spinal cord injury is about people’s lives not expectation. A full life is lived when you make the most of what you have got, not what you have lost…
Tag: neurological level
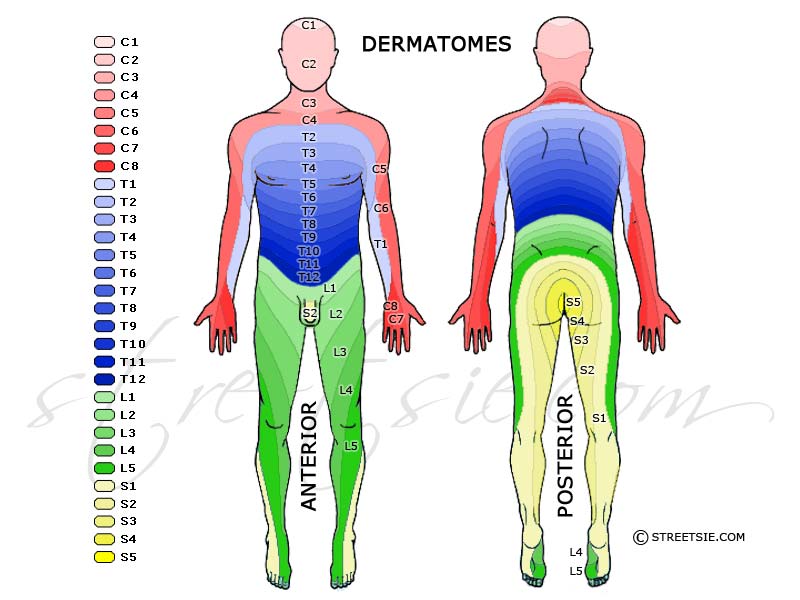
11.4 After spinal cord injury the testing of reflex functions is useful in determining the level and severity of resulting paralysis. Valuable information on the state of the nervous systems can be gathered from testing deep tendon and other reflexes…
11.3 Incomplete means some feeling or muscle function remains below the neurological level of spinal cord injury. Complete means no feeling or muscle function below the neurological level of injury. Neither necessarily affects a persons ability to love and respect, achieve goals, and live a full satisfying life.
11.2 Neurological assessments provide valuable information on the location and extent of spinal cord damage. Additionally a level (T12) and category (complete or incomplete) can be diagnosed from the assessment, useful for rehabilitation and indicative of how much support will be required in order to re-join the community…



Recent Comments