A bladder washout is a technique used to flush blood clots or debris from the bladder by pushing solution into the bladder and immediately draining. A bladder washout may also be performed when unable to drink enough fluids, or to rid the bladder of certain urinary tract infections.
Tag: spinal injury unit
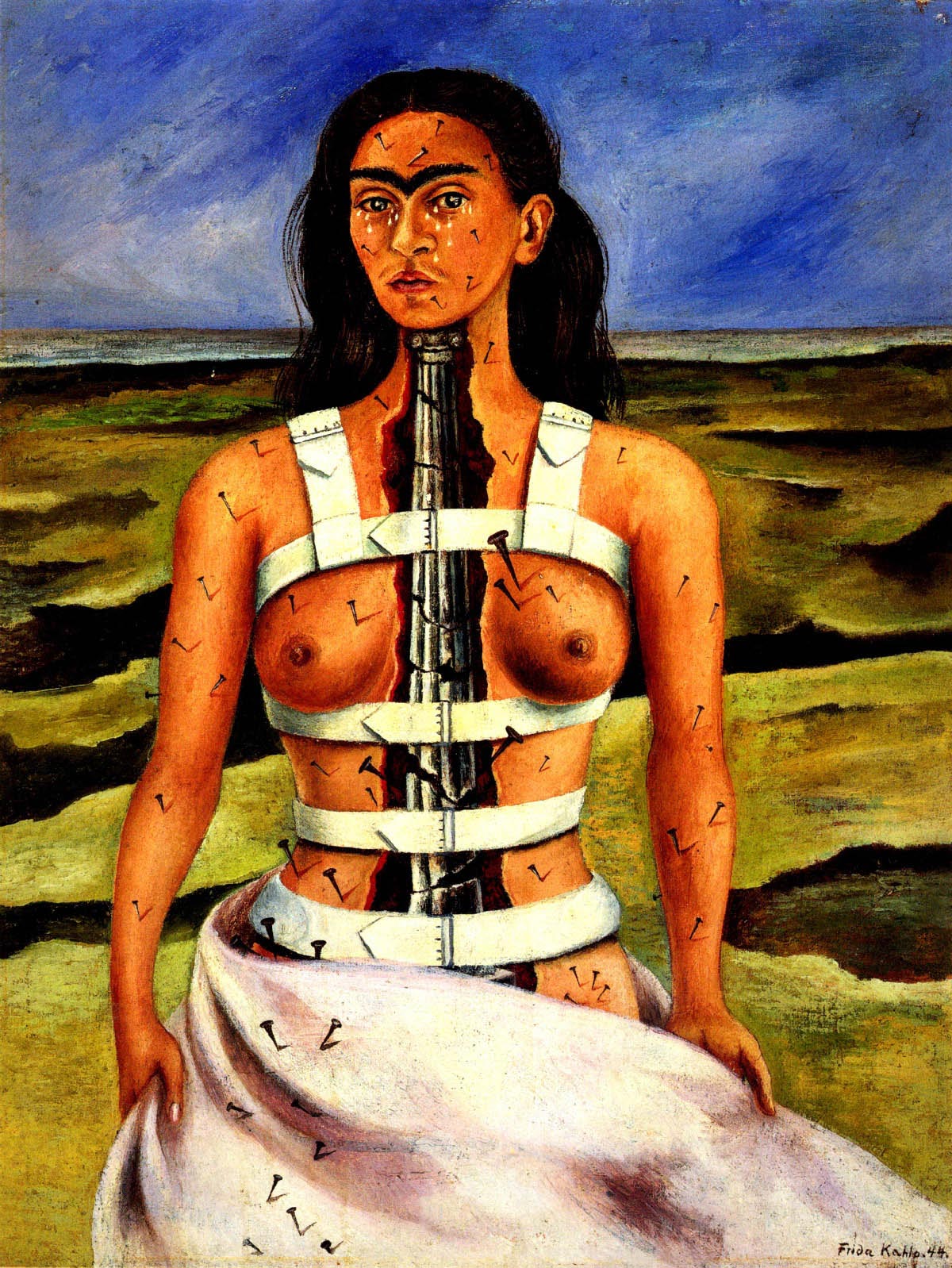
Influential Mexican painter Frida Kahlo (1907-1954) painted images of a disabled female body. Striking self portrait’s of her own trauma following a tram car accident in 1925 in which she suffered spinal column and spinal cord injuries. Frida Kahlo paintings and artworks are an artists journey through pain trauma and recovery.
A National Disability Insurance Scheme will ease the huge financial cost of living with a disability like spinal cord injury. What if it happened to your son, wife or mother. Could you drop your job put your life on hold and meet their care needs for the rest of their life?”
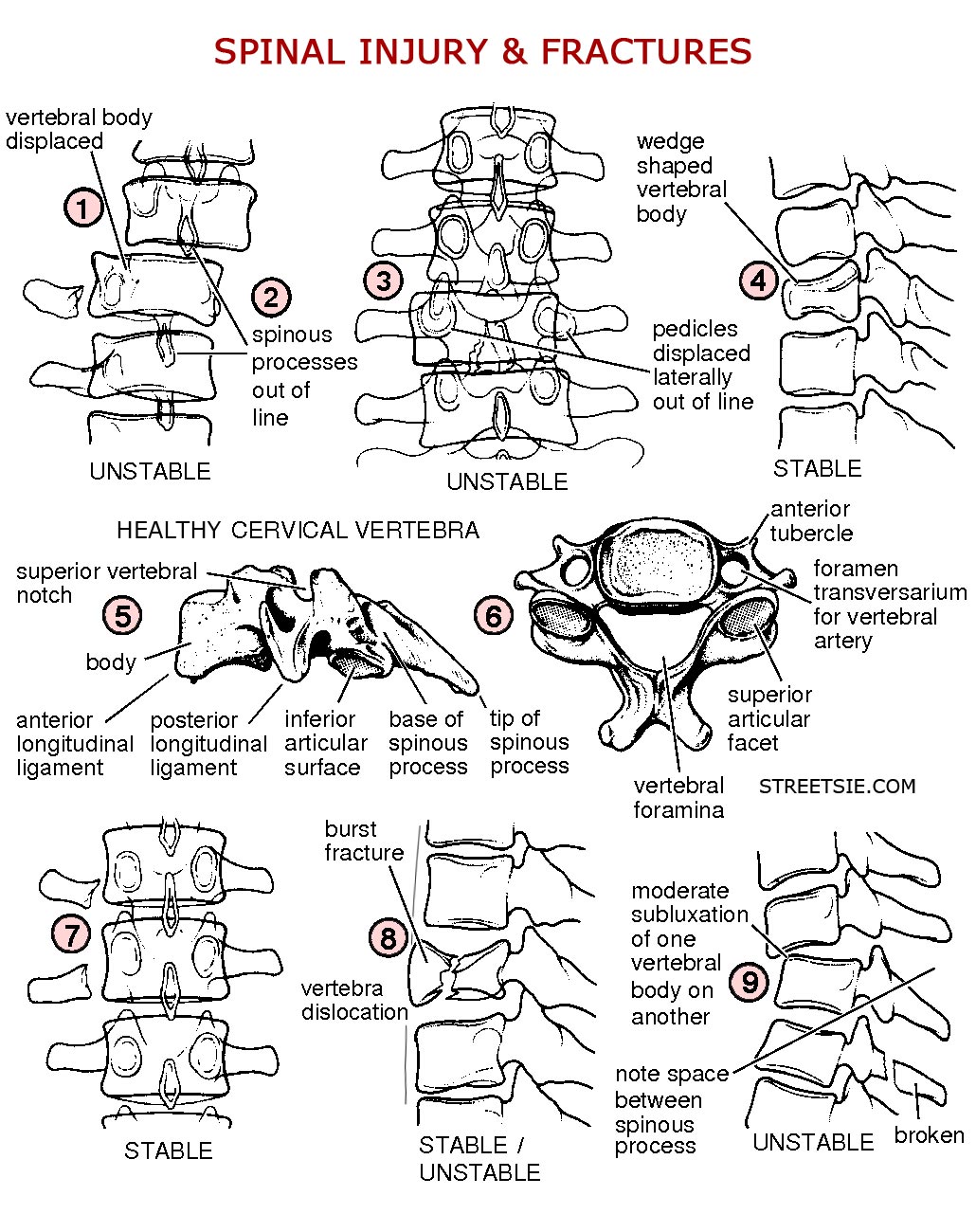
Radiology x-rays offer vital information to medical specialists after a spinal injury. The location and severity of damage revealed by x-rays directly determines the appropriate course of action to achieve best possible short and long term outcomes. MRI and CT scans further identify soft tissue and spinal cord damage.


Recent Comments