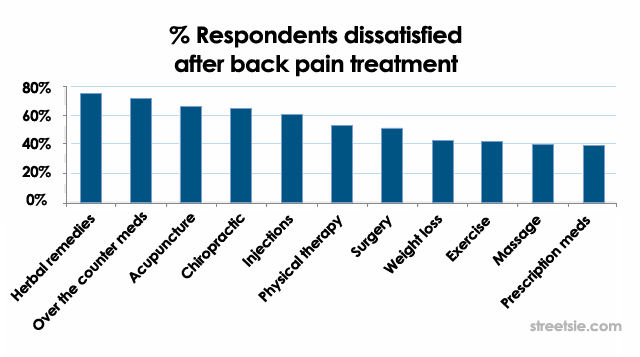
The odds of experiencing chronic pain at some point in our life is extremely high especially after spinal cord injury. Adequate early pain management has proven beneficial to long term chronic pain relief outcomes helping avoid one of the biggest fears related to chronic paiin, addiction to narcotic pain relief medications.
Tag: disability depression
Feminist, author, disability activist, Andrea Rita Dworkin suffered from an agonizing bone disease for many years. She describes her disability with grim humor and shares her worst moments and triumphs in overcoming crippling pain…
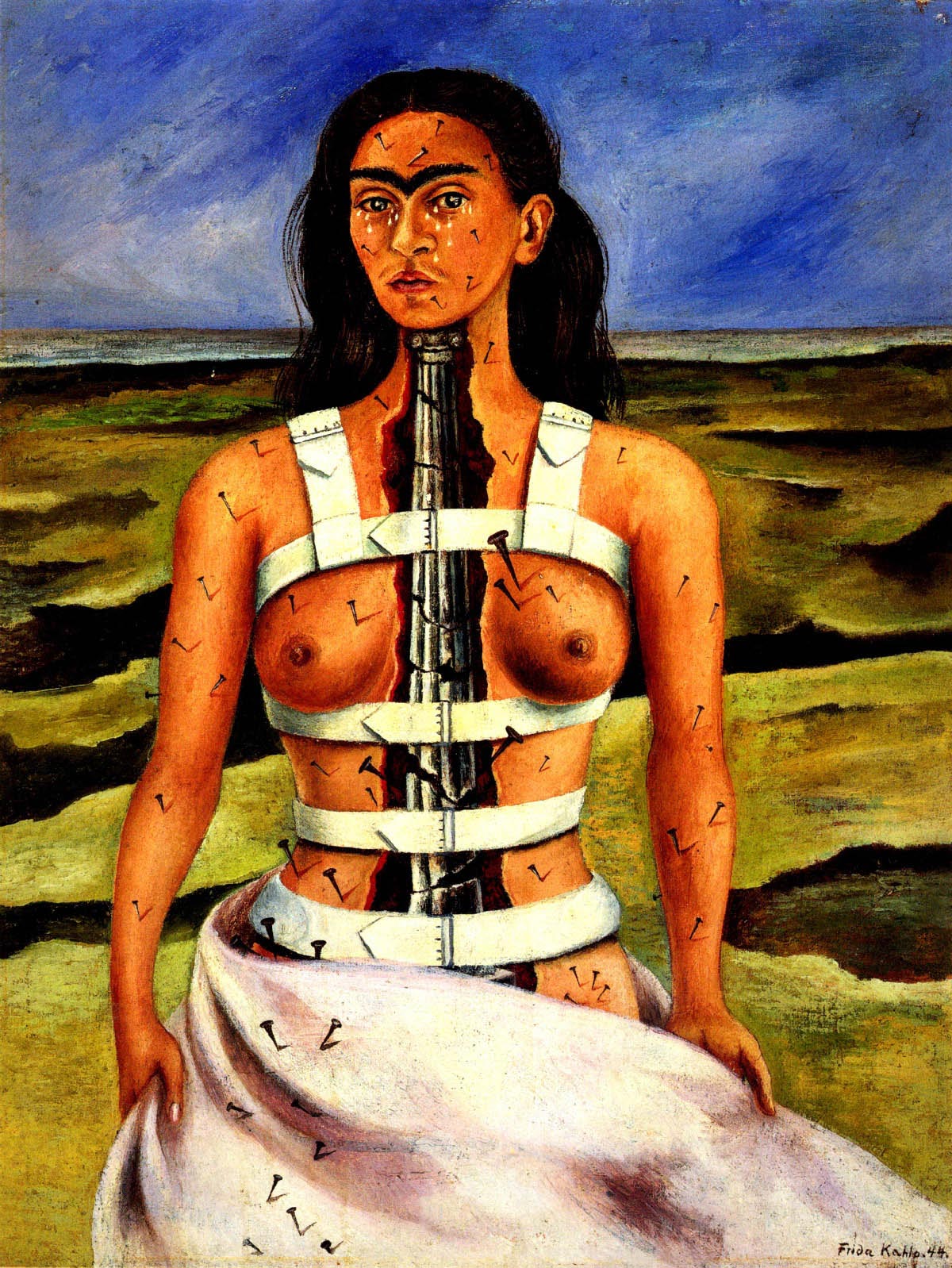
Influential Mexican painter Frida Kahlo (1907-1954) painted images of a disabled female body. Striking self portrait’s of her own trauma following a tram car accident in 1925 in which she suffered spinal column and spinal cord injuries. Frida Kahlo paintings and artworks are an artists journey through pain trauma and recovery.
Depression is not caused by a weakness or lack of will power. After spinal cord injury the incidence rate of depression in both men and women more than doubles. The impact of a traumatic event does not end when people have begun to mend physically. It is also important to note that the passage of time does not always heal the feelings caused by trauma. Often the longer one goes without getting help the more intense the feelings of distress.


Recent Comments